JAMA Intern Med. 2020;180(5):745-752. doi:10.1001/jamainternmed.2020.0403 Published online March 16, 2020.
IMPORTANCE Penicillin allergy is a for patients, antimicrobial stewardship programs, and health services. Validated clinical decision rules are urgently needed to identify low-risk penicillin allergies that potentially do not significant public health issue require penicillin skin testing by a specialist.
OBJECTIVE To develop and validate a penicillin allergy clinical decision rule that enables point-of-care risk assessment of patient-reported penicillin allergies.
DESIGN, SETTING, AND PARTICIPANTS In this diagnostic study, a multicenter prospective antibiotic allergy–tested cohort of 622 patients from 2 tertiary care sites in Melbourne, Australia (Austin Health and Peter MacCallum Cancer Centre) was used for derivation and internal validation of a penicillin allergy decision rule. Backward stepwise logistic regression was used to derive the model, including clinical variables predictive of a positive penicillin allergy test result. Internal validation of the final model used bootstrapped samples and the model scoring derived from the coefficients. External validation was performed in retrospective penicillin allergy–tested cohorts consisting of 945 patients from Sydney and Perth, Australia, and Nashville, Tennessee. Patients who reported a penicillin allergy underwent penicillin allergy testing using skin prick, intradermal, or patch testing and/or oral challenge (direct or after skin testing). Data were collected from June 26, 2008, to June 3, 2019, and analyzed from January 9 to 12, 2019.
MAIN OUTCOMES AND MEASURES The primary outcome for the model was any positive result of penicillin allergy testing performed during outpatient or inpatient assessment.
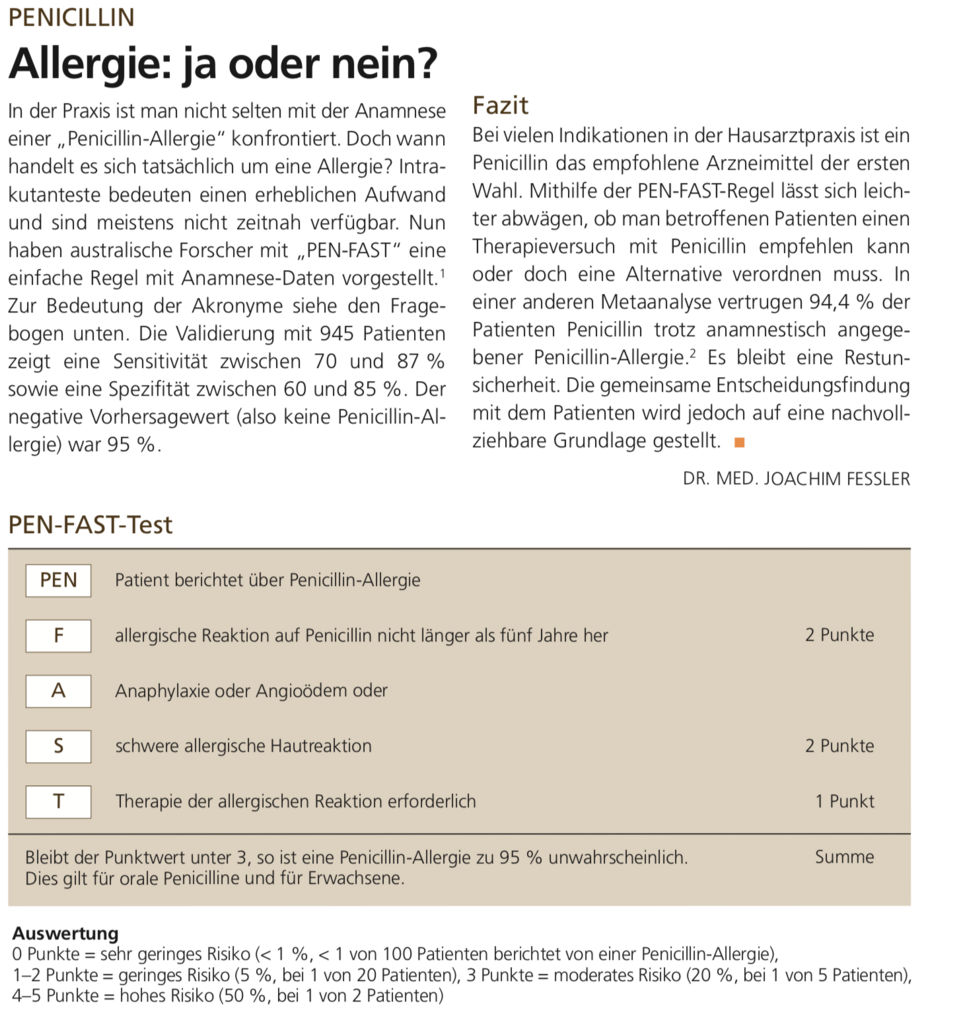
RESULTS From an internal derivation and validation cohort of 622 patients (367 female [59.0%]; median age, 60 [interquartile range{IQR}, 48-71] years) and an external validation cohort of 945 patients (662 female [70.1%]; median age, 55 [IQR, 38-68] years), the 4 features associated with a positive penicillin allergy test result on multivariable analysis were summarized in the mnemonic PEN-FAST: penicillin allergy, five or fewer years ago, anaphylaxis/angioedema, severe cutaneous adverse reaction (SCAR), and treatment required for allergy episode. The major criteria included an allergy event occurring 5 or fewer years ago (2 points) and anaphylaxis/angioedema or SCAR (2 points); the minor criterion (1 point), treatment required for an allergy episode. Internal validation showed minimal mean optimism of 0.003 with internally validated area under the curve of 0.805. A cutoff of less than 3 points for PEN-FAST was chosen to classify a low risk of penicillin allergy, for which only 17 of 460 patients (3.7%) had positive results of allergy testing, with a negative predictive value of 96.3% (95% CI, 94.1%-97.8%). External validation resulted in similar findings.
CONCLUSIONS AND RELEVANCE In this study, PEN-FAST was found to be a simple rule that accurately identified low-risk penicillin allergies that do not require formal allergy testing. The results suggest that a PEN-FAST score of less than 3, associated with a high negative predictive value, could be used by clinicians and antimicrobial stewardship programs to identify low-risk penicillin allergies at the point of care.
Fazit:
Grundsätzlich wird die „Allergie“ wohl überschätzt. Sehr hilfreiches Entscheidungsinstrument um das Risiko einer Penicillinallergie in der Praxis abzuschätzen. Eine Möglichkeit wäre, die Patienten mit der ersten Tablette in der Praxis eine Stunde nach zu beobachten.
Fazit Regen:
Score ist sehr hilfreich.