Jonas Ghouse MD Jonas L. Isaksen MSc Morten W. Skov MD Bent Lind MD Jesper H. Svendsen MD Jørgen K. Kanters MD Morten S. Olesen PhD Anders G. Holst MD Jonas B. Nielsen MD First published: 09 October 2019 https://doi.org/10.1111/dom.13891.Diabetes Obes Metab 2020 Feb;22(2):231-242.
Citations: 2
Funding information: Danish Heart Foundation, Grant/Award Number: 16‐R107‐A6779; Fonden til Lægevidenskabens Fremme; Fondsbørsvekselerer Henry Hansen og Hustru Karla Hansen Født Vestergaards Legat; Hallas‐Møller Emerging Investigator; Karen Marie Jespersen og Datters Legat; the Arvid Nilsson Foundation; The John og Birthe Meyer Foundation; The Lundbeck Foundation, Grant/Award Number: R220‐2016‐1434; The Research Foundation at Copenhagen University Hospital
To investigate the effect of diabetes duration on glycaemic control, measured using mean glycated haemoglobin (HbA1c) level, and mortality risk within different age, sex and clinically relevant, comorbidity‐defined subgroups in an elderly population with type 2 diabetes (T2D).
Methods
We studied older (≥65 years) primary care patients with T2D, who had three successive annual measurements of HbA1c taken between 2005 and 2013. The primary exposure was the mean of all three HbA1c measurements. Follow‐up began on the date of the third measurement. Individual mean HbA1c levels were categorized into clinically relevant groups (<6.5% [<48 mmol/mol]; 6.5%‐6.9% [48‐52 mmol/mol]; 7%‐7.9% [53‐63 mmol/mol]; 8%‐8.9% [64‐74 mmol/mol]; and ≥9% [≥75 mmol/mol]). We used multiple Cox regression to study the effect of glycaemic control on the hazard of all‐cause mortality, adjusted for age, sex, use of concomitant medication, and age‐ and disease‐related comorbidities.
Results
A total of 9734 individuals were included. During a median (interquartile range) follow‐up of 7.3 (4.6‐8.7) years, 3320 individuals died.
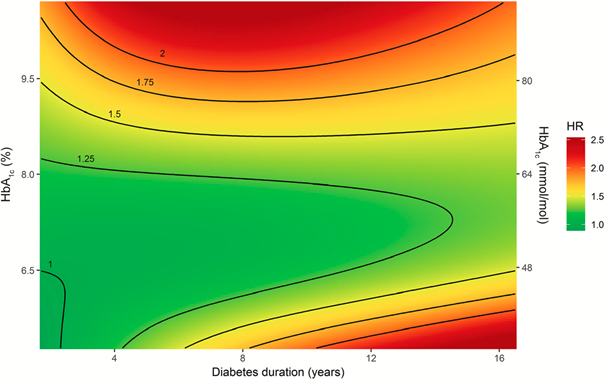
We found that the effect of mean HbA1c on all‐cause mortality depended on the duration of diabetes (P for interaction <.001).
For individuals with short diabetes duration (<5 years), the risk of death increased with poorer glycaemic control (increasing HbA1c), whereas for individuals with longstanding diabetes (≥5 years), we found a J‐shaped association, where a mean HbA1c level between 6.5% and 7.9% [48 and 63 mmol/mol] was associated with the lowest risk of death.
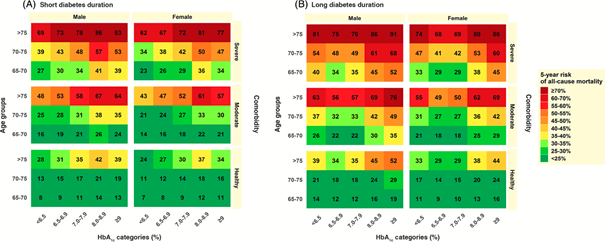
For individuals with longstanding diabetes, both low (<6.5% [<48 mmol/mol]; hazard ratio [HR] 1.21, 95% confidence interval [CI] 1.07‐1.37, P = .002) and high mean HbA1c levels (≥9.0% [≥75 mmol/mol]; HR 1.60, 95% CI 1.28‐1.99, P < .001) were associated with an increased risk of death. We also calculated 5‐year absolute risks of all‐cause mortality, separately for short and long diabetes duration, and found similar risk patterns across different age groups, sex and comorbidity strata.
Conclusions
In elderly individuals with T2D, the effect of glycaemic control (measured by HbA1c) on all‐cause mortality depended on the duration of diabetes. Of particular clinical importance, we found that strict glycaemic control was associated with an increased risk of death among individuals with long (≥ 5 years) diabetes duration. Conversely, for individuals with short diabetes duration, strict glycaemic control was associated with the lowest risk of death. These results indicate that tight glycemic control may be beneficial in people with short duration of diabetes, whereas a less stringent target may be warranted with longer diabetes exposure.
Fazit:
Bei geringerer Diabetesdauer (5 Jahren) führt hier eine strengere Blutzuckereinstellung zur Reduktion der Gesamtmortalität. Patienten, die eine Diabetesdauer von über 5 Jahren haben haben bei HbA1c-Werten zwischen 6,5 und 7,9 die niedrigste Gesamtmortalität. Insbesondere zu niedrige HbA1c-Werte führen zu einer Erhöhung der Mortalität was a.e. auf Hypoglykämien durch z.B SH, die in Dänemark wohl noch mehr eingesetzt werden (13% vs 18%). Lediglich bei sehr hoher Komorbidität kann eine strengere Diabeteseinstellung auch bei längerer Diabetesdauer mit Allgemeinmaßnahmen und Medikamenten ohne Hypoglykämierisiko mit dem Patienten diskutiert werden. Unsere multimorbiden Patienten mit reduzierter Lebenserwartung zählen dazu nicht.
Die Grafik kann wie ein Ampelsystem vielleicht Patienten, die sehr strikt eingestellt sind, helfen, die Medikation auch zu überdenken hinsichtlich Nutzen/Risiko. Nicht immer ist der niedrigste HbA1c der Beste.
Fazit Regen:
Je länger ein Zucker besteht, umso vorsichtiger muss ich mit der strengen Einstellung sein. Zu Beginn einer Zuckererkrankung darf man strenger sein.